- News
- A Brain-Spine Interface Complements Deep-Brain Stimulation – 2nd Place Winner of the BCI Award 2020
A Brain-Spine Interface Complements Deep-Brain Stimulation – 2nd Place Winner of the BCI Award 2020
More than 90% of people with Parkinson’s disease (PD) suffer from gait and balance deficits that reduce quality of life. In the late-stage PD, these deficits respond poorly to commonly available therapies such as sensory cuing, dopamine replacement strategies and deep brain stimulation (DBS). These deficits are associated with disrupted communication between the brain and spinal cord resulting from the depletion of dopaminergic and cholinergic circuits in PD. This project has been submitted for the BCI Award 2020 and has won the 2nd Place of this international BCI competition.
Hi Tomislav, you submitted your BCI research “A Brain-Spine Interface Complements Deep-Brain Stimulation to Both Alleviate Gait and Balance Deficits and Increase Alertness in a Primate Model of Parkinson’s Disease” to the BCI Award 2020 and won the 2nd place. Could you briefly describe what this project was about?
Prof. Gregoire Courtine, who co-directs the NeuroRestore center together with Prof. Jocelyne Bloch and is the lead senior author of the study, displays the main components of the brain-spine interface – a neuroprosthetic system that directly links the brain with the spinal cord in order to alleviate neurological motor deficits. All devices needed for the clinical brain-spine interface are FDA approved for medical use, or have an FDA IDE approval and are currently being used in human clinical trials. Preparations for a clinical trial to demonstrate safety and efficacy of the brain-spine interface in people with Parkinson’s are underway.
Tomislav: “We previously developed a brain–spine interface – a neuroprosthesis that infers movement intentions from cortical activity and then modulates spinal cord stimulation to elicit or reinforce those movements. We used this brain-spine interface to restore walking of non-human primates after paralyzing spinal cord injury. Somewhat similar to spinal cord injury, Parkinson’s disease also disrupts the communication between the brain and spinal cord. As a result, the Parkinson’s disease patients can experience pronounced gait and balance deficits. Cure or effective palliative treatment for these patients is still missing. In this study, we redesigned the brain-spine interface for the application in Parkinson’s disease. We demonstrated that this neuroprosthesis substantially alleviated Parkinsonian gait and balance deficits in a non-human primate model of the disease. Furthermore, we showed that the brain-spine interface synergizes with the deep brain stimulation, which is a standard clinical therapy for late stage Parkinson’s disease patients.”
What was your goal?
Tomislav: “Our goal was to develop and demonstrate a therapy that can alleviate gait and balance deficits of Parkinson’s disease patients, a condition that currently has no treatments.”
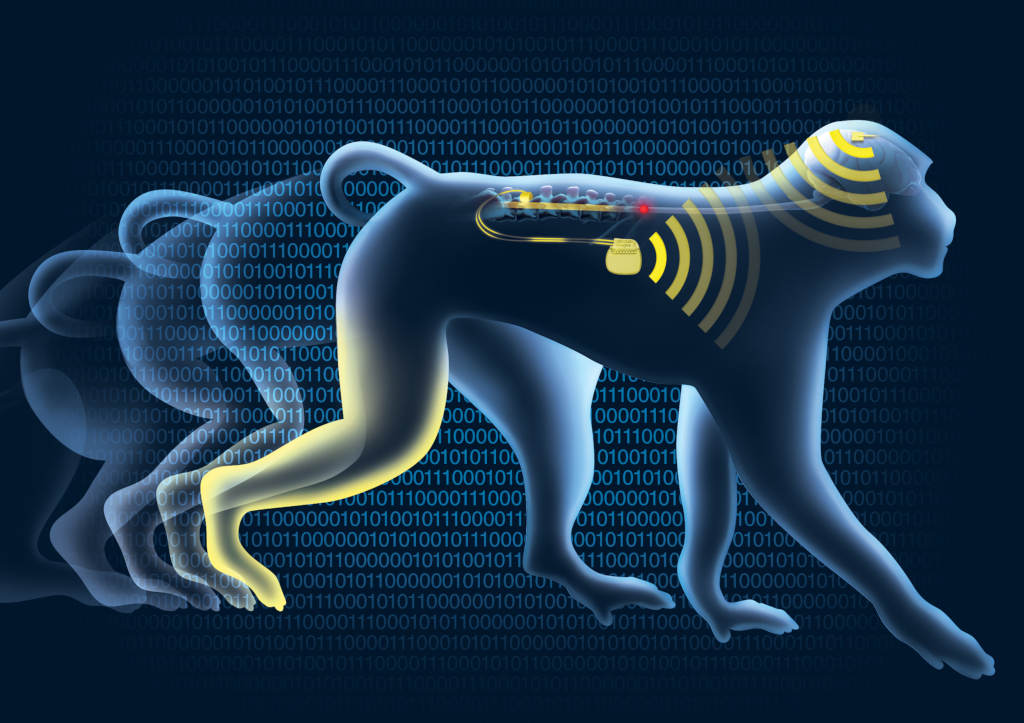
Illustration of the brain-spine interface validated in a non-human primate model of Parkinson’s disease. This neuroprosthesis infers movement attempts from the brain activity wirelessly acquired by a neurosensor. The neuroprosthesis then send wireless stimulation commands to the spinal implant. The spinal implant stimulates the spinal cord to reinforce attempted movements and, therefore, alleviate gait and balance deficits of Parkinson’s disease.
What technologies did you use?
Tomislav: “We assembled a brain-computer interface system that comprised:
- Blackrock microelectrode arrays implanted into the left and right leg motor cortex in order to record action potentials of motor cortical neurons.
- A skull mounted pedestal and a wireless data transmission module used to send the neural signals to an external receiver in order to allow unimpeded behavior of the subjects.
- Blackrock Neural Signal Processor to acquire the wirelessly received neural signals.
- A control computer that ran an in-lab developed software application. This application acquired the neural signals, processed them, inferred the intended movements and then sent out commands to the spinal cord stimulation system to stimulate the spinal cord in a way that reinforces intended movements.
- A Medtronic software application that ran on the control computer that wirelessly relayed the stimulation commands towards the subject.
- A Medtronic Patient Programmer that received the wireless stimulation commands and passed them on to through the skin.
- A Medtronic Activa RC implanted pulse generator that received the stimulation commands and elicited the stimulation.
- Two in-lab designed and fabricated 8-electrode spinal leads implanted over the dura of the lumbosacral spinal cord that delivered the stimulation.
Apart from the spinal lead, which had to be designed specifically for non-human primates in order to fit within the much smaller spinal canal when compared to humans, all other devices are FDA approved for medical use, or have an FDA IDE approval and are currently being used in human clinical trials. We intentionally relied on medical grade devices in order to demonstrate a rapid path towards clinical use of our system.”
The critical components of the brain-spine interface. Right hand. A 96-channel microelectrode Blackrock array is implanted into the phantom of the brain in the area corresponding to the leg motor cortex. These arrays are used to record action potentials of cortical neurons that represent movement attempts. Brain-spine interface acquires these brain signals to infer leg movement attempts. Left hand. Medtronic implantable pulse generator connects to a multielectrode lead to form a spinal implant. Brain-spine interface uses inferred movement attempts to wirelessly control the spinal implant in real time. The spinal implant stimulates the spinal cord in order to reinforce the attempted movements, and therefore alleviate gait and balance deficits of Parkinson’s disease.
What kind of people could benefit from your research?
Tomislav: “People with Parkinson’s disease that develop gait and balance deficits. These deficits are common at the late stage of the disease and are one of the lead causes of injury for Parkinson’s disease patients. Both the deficits and the injuries that result from them severely impact the quality of life for these patients.”
Do you think your work as future potential for clinical use?
Tomislav: “Our brain-spine interface relied on medical grade devices. This gives us a clear path towards clinical trials and subsequent use of the technology around the world. We are currently preparing applications for regulatory approval to conduct the first-in-human clinical trials with a therapy system that was derived from the brain-spine interface described in our project. We are looking forward to demonstrating the efficacy of this system in patients with Parkinson’s disease in the near future.”
How was it to win the second place in the BCI Award 2020?
Tomislav: “Exhilarating. I’ve spent my whole research carrier (10+ years) in the BCI field and was elated to receive a recognition of my work from the BCI research community. Equally important, it was great to meet with the BCI community, especially since this year’s BCI social at the SFN conference could not be held. I do hope to see everyone again in the coming years.”
How can students, researchers get involved in your research?
Tomislav: “My host institution, the Defitech Center for Interventional Neurotherapies – NeuroRestore – is engaged in several cutting-edge BCI clinical trials. The center is nested in Lausanne, Switzerland that features beautiful views over the Lake Geneva and amongst the highest academic salaries worldwide. We have several open positions and are very much open for collaborations. They can find more details at www.neurorestore.swiss.”
A brain–spine interface complements deep-brain stimulation to both alleviate gait and balance deficits and increase alertness in a primate model of Parkinson’s disease
Tomislav Milekovic1,2,3,4, Flavio Raschellà1,2,3,5, Matthew G. Perich2, Eduardo Martin Moraud1,2,3,6, Shiqi Sun1,2,3,7, Giuseppe Schiavone8, Yang Jianzhong9,10, Andrea Galvez1,2,3,4, Christopher Hitz1, Alessio Salomon1, Jimmy Ravier1,2,3, David Borton1,11, Jean Laurens1,12, Isabelle Vollenweider1, Simon Borgognon1,2,3, Jean-Baptiste Mignardot1, Wai Kin D Ko9,10, Cheng YunLong9,10, Li Hao9,10, Peng Hao9,10, Laurent Petit13,14, Qin Li9,10, Marco Capogrosso1, Tim Denison15, Stéphanie P. Lacour8, Silvestro Micera5,16, Chuan Qin10, Jocelyne Bloch1,2,3,6, Erwan Bezard9,10, 13,14, Grégoire Courtine1,2,3,6
1 Center for Neuroprosthetics (CNP) and Brain Mind Institute, School of Life Sciences, Swiss Federal Institute of Technology (EPFL), Switzerland
2 Department of Clinical Neuroscience, Lausanne University Hospital (CHUV) and University of Lausanne (UNIL), Switzerland
3 Defitech Center for Interventional Neurotherapies (NeuroRestore), CHUV/UNIL/EPFL, Switzerland
4 Department of Fundamental Neuroscience, Faculty of Medicine, University of Geneva, Switzerland
5 CNP and Institute of Bioengineering, School of Engineering, EPFL, Switzerland
6 Department of Neurosurgery, CHUV, Switzerland
7 Beijing Engineering Research Center for Intelligent Rehabilitation, College of Engineering, Peking University, People’s Republic of China
8 CNP, Institute of Microengineering and Institute of Bioengineering, School of Engineering, EPFL, Switzerland
9 Motac Neuroscience, UK
10 Institute of Laboratory Animal Sciences, China Academy of Medical Sciences, People’s Republic of China
11 Carney Institute for Brain Science, School of Engineering, Brown University, USA
12 Department of Neuroscience, Baylor College of Medicine, USA
13 Université de Bordeaux, Institut des Maladies Neurodégénératives (IMN), UMR 5293, France
14 CNRS, IMN, UMR 5293, France
15 Oxford University, UK
16 The BioRobotics Institute, Scuola Superiore Sant’Anna, Italy