

- News
- How Can We Train The Brain To Help Stroke Patients?
How Can We Train The Brain To Help Stroke Patients?
Many people who have had a stroke have trouble moving, even after therapy with the best experts and methods. New ways to make stroke therapy more effective could help people recover more effectively. Some research groups have developed brain-computer interface (BCI) systems that can measure when a stroke patient imagines hand movement by recording brain waves. We developed a BCI that used each patient’s brain activity to control a muscle stimulator and a monitor during therapy. The patients got rewarding feedback during therapy when they imagined a movement correctly. We tested 51 patients, some of whom had a stroke many years ago. Forty nine patients improved after the therapy, based on the results of standardized tests. Therefore, BCI-based therapy could help some stroke patients. We think there will be further advances in the next several years that will lead to more effective therapies using BCIs.
WHAT HAPPENS WHEN A PERSON HAS A STROKE?
A stroke is a type of brain damage that is becoming more common because people are living longer. A stroke happens when a blood vessel in the brain is blocked or starts to bleed. In either case, some parts of the brain do not get the blood supply that they need, which can cause serious brain damage. After a stroke, it is important that the patient gets to a hospital immediately. Doctors can sometimes help patients recover from some of the brain damage within a few days after the stroke. However, even with hospital treatment, many patients have serious, long-lasting brain damage and need extensive therapy.
OPEN YOUR OWN RECOVERIX CENTER
The brain consists of two halves, called the left and right hemispheres. Usually, a stroke only affects one hemisphere, so some stroke survivors have trouble moving the left or right side of the body. In severe cases, a patient’s arm and leg on the left or right side may be completely paralyzed. In many milder cases, patients only have trouble with an arm or leg (not both) and can perform almost all movements normally. Stroke can cause another problem called spasticity. This means that some muscles are too tense. Patients might have pain, difficulty moving, unintended movements, and other problems.

Difficulty with movement can lead to many challenges. Stroke survivors might not be able to work or enjoy their favorite sports or hobbies. They might need help from friends and family, and they may have financial trouble from lost work and the costs of treatment and care. Some stroke survivors are uncomfortable being in public because they think people will tease them about their disabilities. These are only some reasons why we need the best possible approaches and technologies to help stroke patients recover the ability to move.
HOW CAN BCI TECHNOLOGY BE USED TO TREAT STROKE PATIENTS?
Imagine a stroke patient who is no longer able to move one hand. To treat stroke patients, therapists often ask the patient to imagine or attempt certain kinds of hand movements. Over dozens of therapy sessions, this helps the brain relearn how to control the affected hand. A measurement called an electroencephalogram (EEG) has been used for many years to measure the brain’s electrical activity [1]. This technique uses little metal discs called electrodes, which are placed on the head. The EEG can tell us which areas of the brain are active. For example, by placing electrodes over the brain areas responsible for movement and sensation, we can study the brain activity that happens when a person moves or feels a sensation.

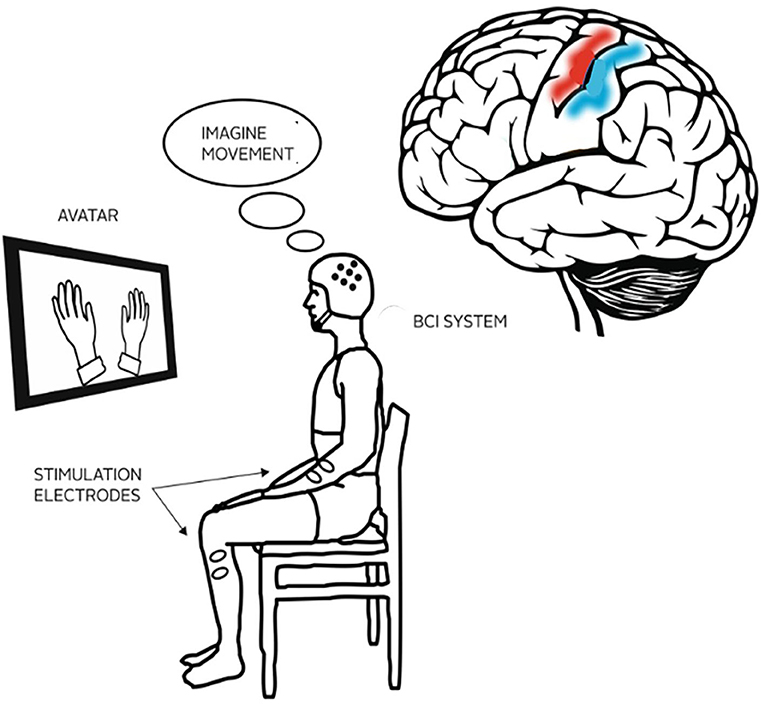
EEG can be combined with a brain-computer interface (BCI) to create a new kind of stroke therapy. A BCI is a system that can provide real-time feedback about the brain’s activity to the person receiving therapy. The BCI system can detect when patients imagine the correct hand movements and can let the patients know whether those movements are correct. For example, if the patient imagines a left-hand movement, then a cartoon hand on the monitor might mimic that movement, while a muscle stimulator helps the left hand to move. This way, the patient only gets rewarding feedback from the system while performing the imagined movement correctly. Seeing a cartoon hand move while also feeling their own hands move can help motivate patients and encourage their brains to relearn motor functions. Many other types of BCIs have been developed. Using BCIs in post-stroke therapy can lead to increased brain plasticity, meaning that the brain can create new connections that help it learn to perform certain functions again, such as moving the hand without spasms or other difficulties.
TESTING BCI IN STROKE PATIENTS
We asked 51 patients to participate in our study. These patients were 61 years old, on average, and had their strokes an average of 37 months prior to the study. Some people believe that patients who had strokes more than 12 months ago will probably not improve, but we hypothesized otherwise.
The patients participated in two pre-assessments before the therapy. In the pre-assessments, we conducted tests to study each patient’s motor skills and other factors. Pre-assessments were done on 2 different days, separated by 1 month, to ensure we had a good understanding of the abilities of the patients before the therapy. Then, the patients participated in 25 to 31 BCI therapy sessions with a licensed therapist. Each session lasted about 1 h, and most patients did 2 sessions per week (Figure 1). Afterwards, we did three post-assessments to study how each patient changed. The first post-assessment was done immediately after the last therapy session, and other post-assessments were done 1 and 6 months later.
WHAT DID WE MEASURE?
We explored the effect of BCI therapy by measuring three separate factors:
- BCI accuracy
- Brain activity
- Movement
BUY RECOVERIX FOR YOUR HOSPITAL
BCI accuracy is a way to measure each patient’s engagement in the motor imagery tasks. High BCI accuracy indicates that the patient is paying attention to the tasks and imagining the movements correctly. If the patient does not imagine any movement, then BCI accuracy will be around 50%. Therefore, low accuracy might indicate that the patient is not participating or is not imagining movements correctly. A therapist might then coach the patient to help him or her improve BCI accuracy (Figure 2A).
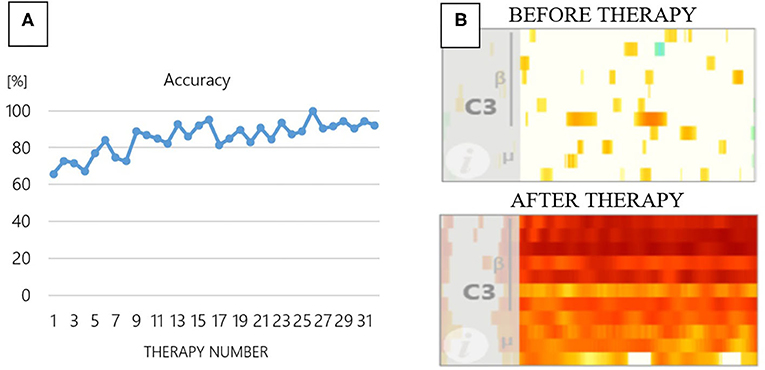
Figure 2 – (A) BCI accuracy from therapy sessions 1 through 31 for one patient. At first, the BCI accuracy when classifying left- vs. right-hand movement was 65%. The accuracy improved with additional therapy sessions and reached 100% in session 25. (B) Brain activation before and after 31 sessions of BCI therapy. The white color before therapy indicates that there is no brain activation to produce hand and finger movements, while the red color after therapy indicates more brain activation. C3 is the name of the electrode position over the brain area responsible for right-hand movement.
Brain activity is measured throughout BCI therapy. Usually, in the early therapy sessions, the movement areas of the brain are not working together effectively. Over the weeks of therapy, we often see that the movement areas in the brain become much more active (Figure 2B). The colors in Figure 2B indicate the brain activation at different frequencies over areas that are important for movement. The x-axis indicates the time in each trial; areas further to the right indicate later times in the trial. The y-axis reflects different frequencies. The lower areas of the graph are lower frequencies (indicated by the Greek letter mu) and the higher areas of the graph are higher frequencies (indicated by the Greek letter beta).
You are currently viewing a placeholder content from Youtube. To access the actual content, click the button below. Please note that doing so will share data with third-party providers.
The most important effect of BCI therapy is helping patients regain movement. Figure 3A shows a tool that therapists and scientists use to test wrist and hand movement, called the Nine-Hole Peg Test because the patient must pick up nine little pegs and put them into nine little holes. We asked patients to perform this test with both hands several times throughout the therapy process and we tracked the time it took them to complete the test. If BCI therapy helped a patient to regain movement, we saw a decrease in the time it took that patient to complete this test over the course of the therapy sessions (Figure 3B).
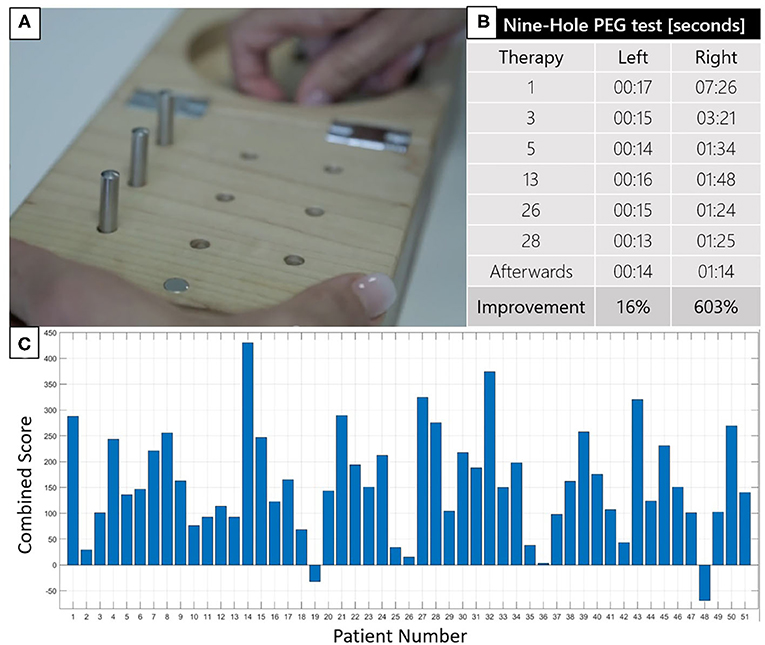
Figure 3 – (A) The Nine-Hole Peg Test can be used to test wrist and hand movement.(B) Results showing improvement of one patient’s hand movement during BCI therapy. The time to complete the task with the affected (right) hand decreased from 7 min 26 s at the start of therapy to 1 min 14 s after 28 therapies. (C) Summary of all motor function tests, combined, for all patients studied. If the bar is above zero, movement was improved after the therapy. Forty nine patients showed improvements, while only two patients showed decreased movement (one had another stroke and the other did not pay attention).
WHAT DID WE LEARN FROM OUR STUDY?
We used many tests in addition to the Nine-Hole Peg Test to measure pain, spasticity, concentration, memory, and how well patients could perform different movements with and without help. Some tests were just questionnaires that asked about daily activities, such as whether the patient could put on a T-shirt without help. We conducted 18 tests with every patient, and a higher combined test score indicated a greater improvement in these tests (Figure 3C). Our results showed that the BCI therapy helped most patients regain movement and/or reduce spasticity in their hands and arms. We found that the therapy works better for patients who achieve more than 80% accuracy. BCI therapy even worked many years after the patient’s stroke. One patient participated 31 years after the stroke and still improved! Our results told us that BCI therapy helped the patients’ brains to learn how to better control their movements.

This article has been published in Frontiers For Young Minds, October 1, 2021.
Glossary
- Hemispheres: The right and left halves of the brain. The left hemisphere controls movement on the right side of the body, and vice versa.
- Spasticity: This disorder can include spasms (involuntary movements), stiff or tight muscles, pain, and overactive reflexes. People may have trouble with posture, walking, typical daily activities, and other movements.
- Electroence-Phalogram (EEG): A measurement of the natural electrical activity produced by the brain, obtained using electrodes placed on the head.
- Electrodes: Small sensors that detect brain activity. EEG electrodes are generally small, metal disks mounted in a cap, which do not penetrate the skin nor cause pain.
- Brain-Computer Interface (BCI): System that uses direct measurements of brain activity to provide communication and control in real-time. Most BCIs use EEG to measure brain activity.
- Motor Function: The ability to move parts of the body.
- Brain Plasticity: The brain’s remarkable ability to change itself to adapt to new information and situations, such as therapy. This ability helps people recover from stroke and other injuries.